Setting the Stage
Manual medical claims auditing has long since and will remain, a highly specialized engine of cross-examination, driven by immensely talented auditors and revenue integrity specialists. They are the workforce that keeps hospitals financially viable, protecting their institution from insurance takebacks and securing revenue to prevent costly leakage. In a world that is rich with institutional mergers and acquisitions, revenue integrity specialists and claims auditors are finding themselves responsible for a growing number of providers, claims, and billing compliance scenarios. With the Office of Inspector General (OIG) and commercial payers both aggressively auditing institutions (often armed with augmented and artificial intelligence), it’s time to reexamine the age-old institution of manual medical claims auditing.
What has worked in the past is no longer working for today’s healthcare organizations. What follows is an evaluation of the manual medical claims auditing system, its key inefficiencies, and its potential for change.
A Word on Resources
The true culprit of any overtaxed, inefficient status quo process is often a lack of resources. While it’s apparent that medical claims auditing is chronically plagued by a lack of time and staff (qualified auditing and revenue retention specialist staff are always in demand), conventions make inefficient use of both. Below are three key areas that are affected by the inefficiencies of manual medical auditing, and their negative externalities
Insufficient Sampling
As health groups increase in size and the number of external audits rises, it’s important to understand which services are being inappropriately coded, and where revenue leakage and takebacks are most prevalent. When conducting randomized medical claims audits manually, limited resources and time dictate a relatively small sample size compared to an institution’s total claims. While there may be thousands of claims and codes produced monthly in a single institution, randomized manual auditing results in a small fraction of those being critically examined (the OIG recommends a sample of 5 to 10 charts per provider for a multiple-provider audit).
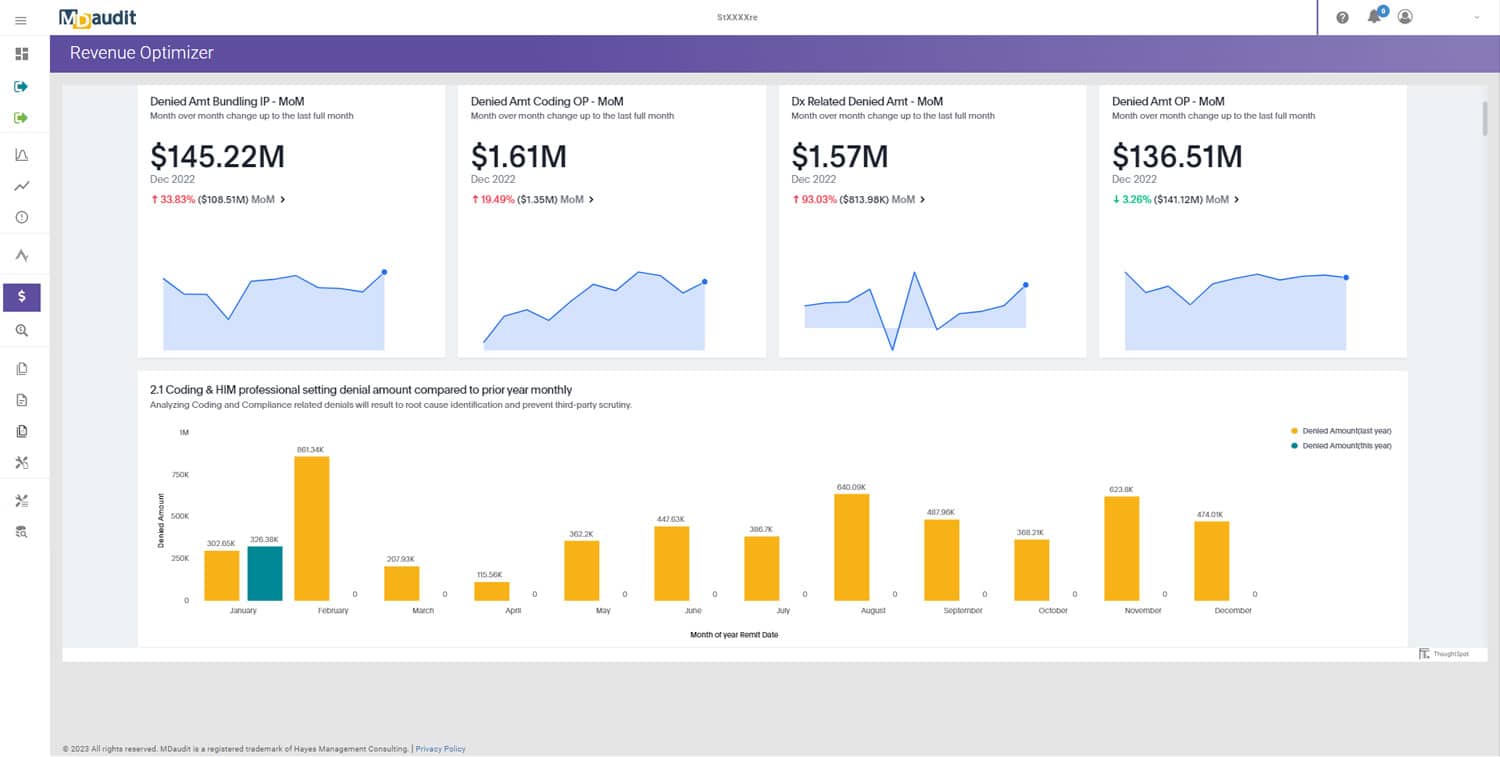
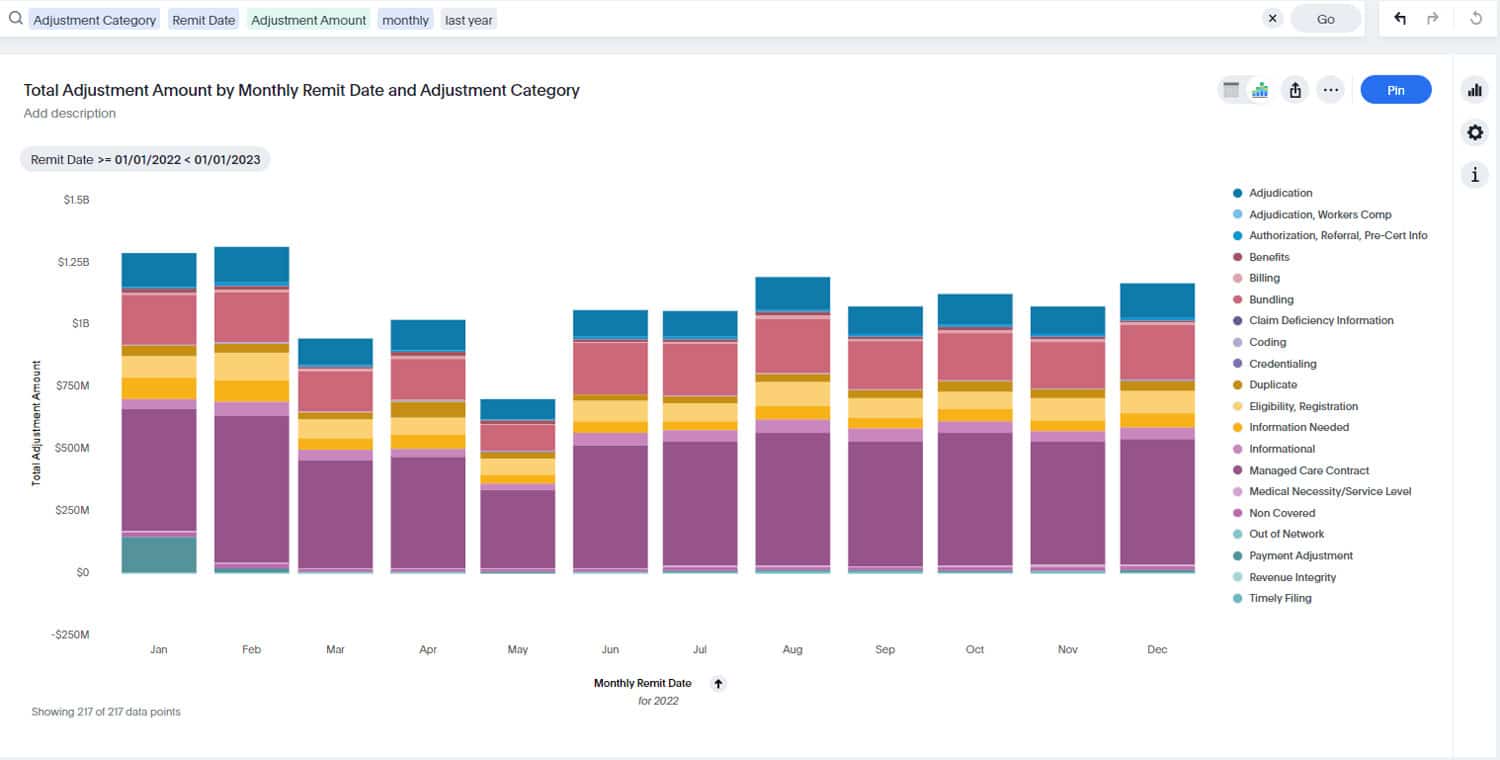
So while manual auditing does restrict the capacity of auditors, it does nothing to support data-driven risk-based auditing. Using automated medical auditing software with analytics, auditors and revenue integrity specialists can harness data to attack larger swaths of internal data for those at the highest historical risk for denials.
Poor Opportunities for Corrective Action Education
Healthcare provider education is an essential part of sealing revenue within an institution and preventing miscoding. A recent study showed that surveyed hospitals discovered their providers were only coding correctly 30% of the time. Auditors and revenue integrity professionals are an essential line of defense for catching these mistakes, identifying the trends, and implementing corrective action. However, when these people have too much on their plate, they cannot spend time with providers performing corrective action education to ensure mistakes are not repeated systemically.
By automating aspects of the medical claims auditing process, auditors and revenue integrity specialists will be empowered to more accurately and quickly identify coding and billing trends and preemptively prevent them through education.
Overtaxed Staff
Finally, manual medical auditing is a tremendous burden on the most valuable element of the medical claims auditing and revenue integrity process: staff. This process is already highly detailed, often tedious, and very high stakes. Conducting claims audits and evaluating for revenue integrity manually makes it as hard as possible for auditors and revenue integrity professionals. Combing through mountains of records detracts from time better spent analyzing and educating. Medical auditing software helps revenue integrity professionals avoid takebacks from both governmental and private insurers, retain revenue within the organization, and protects their time, empowering them to better address systemic inconsistencies and mistakes.
With over $37 billion recovered from individuals and companies by HHS and the OIG in the past decade, It’s important that these professionals focus on compliance and optimizing their institutions, not digging for data.
What’s Broken and What’s Not?
The fact is that auditors serve an invaluable role in protecting their institutions and supporting their financial viability. With proven medical auditing software available and even officially recommended by AAPC, there is little reason for manual medical auditing to continue hindering their performance abilities. Medical auditing software cannot and will not replace the skill and subjectivity of trained medical claims auditors and revenue compliance experts — rather, it is an invaluable tool to improve their efficacy.
By recruiting the power of medical auditing software, medical claims auditors and revenue integrity specialists can continue performing their essential functions at a higher level, supporting and fortifying their institutions and providers.
Click here to explore MDaudit’s suite of audit software services.